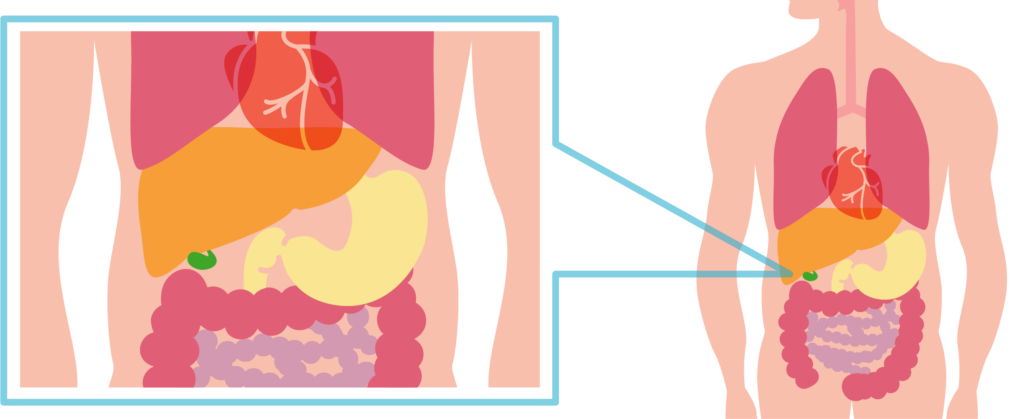
The gall bladder is a small pear-shaped organ resting under your liver (under your right ribs). The gallbladder collects and stores bile (digestive juices) produced by the liver.
The gallbladder is usually removed if it contains gallstones that cause symptoms. These symptoms commonly include recurring pain, inflammation and indigestion. Removal of the gall bladder does not usually impair the digestive system and digestive juices will continue to flow through the bile ducts.
Generally once the gall bladder is removed the symptoms you have had will resolve. In some instances they remain for a short time and then get better. In other cases some symptoms may be due to other conditions (not caused by the gallstones). If you continue to have symptoms (for longer than three months) you should discuss this with your surgeon or GP.
Laparoscopy is commonly known as keyhole surgery and is performed by passing a tiny tube shaped telescope into your tummy. This tube (known as a Laparoscope) is connected to a high intensity light and a video camera so that the surgeon can see what is happening inside you.
This is the medical term for removal of the gall bladder. To remove the gall bladder, four little puncture wounds are made (one in the belly-button, one in the upper abdomen and two under your ribs on the right hand side). Occasionally, a fifth puncture wound is made so that the surgeon can examine the digestive ducts a little closer. A Laparoscope is passed into one of these incisions, and tiny surgical instruments are passed into the others. To provide space for the surgery to be performed, your tummy is filled with carbon dioxide (a harmless gas). Once the gallbladder is freed, it is removed through one of the puncture wounds. The whole procedure normally takes 40-60 minutes.
It is important to note that in about 5 in 100 cases the gallbladder cannot be safely removed by keyhole surgery. There are several reasons for this including people who have had previous operations in their abdomen, unexpected difficulty in removing the gallbladder, severe inflammation, or the risk of damage to surrounding structures. In these cases, the surgeon will need to proceed to an “open” cholecystectomy. This is a bigger procedure and involves making a 10-15 cm incision in your abdomen and will mean a hospital stay of several days. In view of the small chance of needing “open” surgery you will be asked to consent to both techniques. Your recovery period after the open procedure will be longer, so you will need to bear this in mind in relation to return to work and booking/taking of holidays. We will be happy to advise on any of these issues.
All surgery has some risks, and complications occur in about 5 in 100 cases. Most complications are mild and easily resolved. Injuries to the internal structures and organs are rare occurring in up to 6 in 1000 cases. This may require corrective action or further surgery. This will be discussed with you in more detail by the medical team.
Whilst most of these complications are immediately obvious and can be corrected, some may not appear for a few days. There is an increased risk of postoperative complications if you are overweight or if you smoke. The risks of surgery are assessed on an individual basis, as they can vary depending if you have any underlying health issues. Please discuss this with your surgeon
There are no other effective, safe, durable and widely accepted alternatives to surgery. Although other methods have been attempted such as drugs or lithotripsy (the use of shock waves or ultrasonic waves to crush the gall stones), they have not been very successful and gallstones frequently reappear.
The other alternative is to have no treatment. The risks of not treating a diseased gallbladder are repeated attacks of pain and inflammation that may lead to life threatening infections and complications.
Your risk for DVT will be assessed on the day of your operation and you may require an injection of medicine to prevent blood clots. In addition you may be asked to wear anti-embolic stockings that should ideally be worn until you are back to your usual level of activity (usually 24 hours). If you need to wear them for longer than 24 hours, you should remove them for 30 minutes each day. If possible, avoid long periods of immobility, if you feel more tired than usual it is still important that you try to move around to promote circulation. For instance moving around the house or going for short walks.
Your blood pressure, pulse and wounds will be monitored closely over the first few hours. You will normally be able to start drinking shortly after the procedure, and can start eating as soon as you are hungry. You will be able to get out of bed as soon as you feel well enough to although the nurses may assist you the first time.
You may experience some pain from your wounds. If you do, the nurses will give you painkillers.
In addition, you may notice some shoulder pain which is due to the gas inserted into your tummy during surgery. This gas will gradually disappear but the discomfort may persist for several days. Moving around as soon as possible will help prevent gas pains. Before your discharge you will be given a supply of painkillers, dressings and post-operative instructions. Your GP will be notified of your discharge.
A hospital follow-up appointment will be arranged for you
This will be determined during your pre operative assessment.
You would normally come into hospital on the day of your surgery and go home the same day unless there are specific reasons for you to be in hospital the day before your operation.
Whilst most of the effects of anaesthesia wear off in a few hours, it is common to have poor concentration and memory for the first day or so. It is important therefore that you do not make important decisions, sign legal documents or operate machinery or equipment for at least 24 hours after the anaesthetic. Muscle aches or headaches may also be experienced over the first few days.
Nausea and vomiting are not unusual after surgery, we try to keep this at a minimum. Medication can be used during and after the anaesthetic to control this.
Take extra rest and try to drink something regularly. If you can tolerate food, take small frequent snacks.
It is normal to have wound pain after surgery and your tummy may feel quite bloated and tender. This should start to subside after a few days. After about 10 days most of the soreness should disappear. You may also notice that you have a slightly sore throat. This is due to the “breathing” tube placed in your throat during surgery and should subside in a day or so.
To minimise discomfort, you should take the painkillers that you have been given, regularly over the first few days (ensuring that you do not exceed the dose prescribed). After your discharge, if you have any queries or problems with your painkillers you can seek advice from your local GP or chemist.
You can return to normal physical and sexual activities when you feel comfortable. It is normal to feel tired after surgery, so take some rest, two or three times a day, and try to get a good night’s sleep. After a week or so, you should be able to resume most of your normal daily activities. You should avoid heavy lifting and vigorous exercises for at least two weeks.
Before driving you should ensure that you can perform a full emergency stop, have the strength and capability to control the car, and be able to respond quickly to any situation that may occur. Please be aware that driving whilst unfit may invalidate your insurance.
You can return to work as soon as you feel well enough. This will depend on how you are feeling and the type of work that you do. If you have a desk job you may feel ready to return in a week or so. If you are involved in manual labour or heavy lifting you may require a bit more time. Typically, you will need between two and three weeks off work.
There are no dietary restrictions after removal of the gall bladder and you may resume a normal diet as soon as you are hungry. It would be wise to avoid eating fatty food
(e.g. cheese, full fat milk, cream, fried foods) for the first week or so, we would encourage eating a healthy well balanced diet at all times. It may take a few days before your appetite returns. When you feel hungry start with light frequent meals and then increase at your own pace.
You may find it takes three or four days to have a normal movement. If you have not had a bowel movement three days after surgery, a mild laxative should help. If you do not have any laxatives at home your local chemist will be able to advise you. Alternatively, you may experience some diarrhoea after surgery. This should settle within three or four weeks. If the diarrhoea is bothersome your local chemist can advice you on over-the-counter remedies. Remember to drink plenty of fluids so that you don’t get dehydrated.
If you have any concerns or feel unwell once home after the operation, please contact the Surgical Assessment Unit (SAU) on 01274 364413 to speak with a member of the medical team who will offer advice. The department is open 24 hours a day.
When you are in hospital it is essential to wear a wristband at all times to make sure you are safe during your stay. The wristband will show accurate details about you on it including all the information that staff need to identify you correctly and give you the right care.
If you do not have a wristband whilst in hospital, then please ask a member of staff for one. If it comes off or is uncomfortable, ask a member of staff to replace it.
You can contact us using the Relay UK app. Textphone users will need to dial 18001 ahead of the number to be contacted.
Bradford Teaching Hospitals NHS Foundation Trust is a smoke-free organisation. You are not permitted to smoke or in use e-cigarettes in any of the hospital buildings or grounds.