
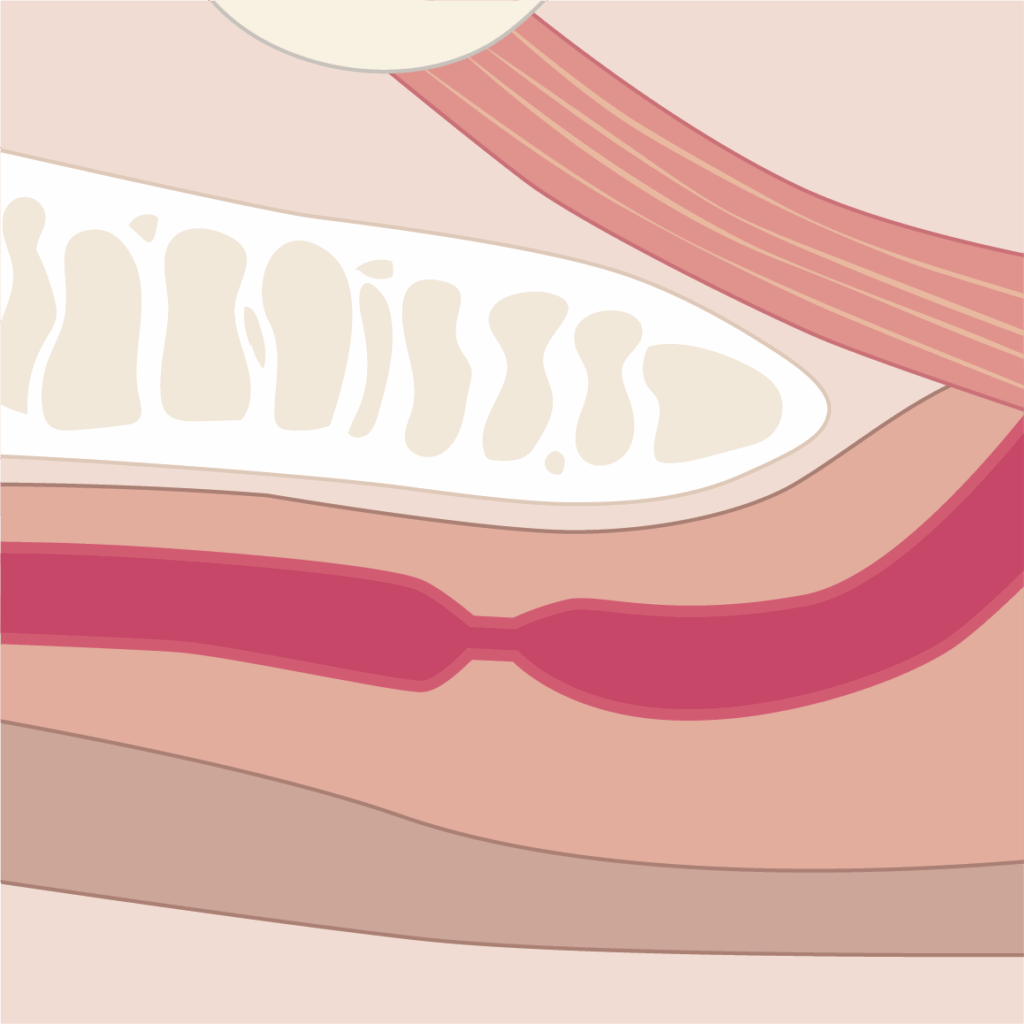
An anterior urethral stricture is a narrowing of the urethra caused by scarring, which obstructs the flow of urine. It is typically identified during a cystoscopy and is located near the beginning of the urethral pipe which brings the urine out of the bladder. Common symptoms include:
Following diagnosis, after your cystoscopy, you will have a consultation with a specialist to discuss your treatment options, as follows:
During this consultation, you will discuss potential side effects of the treatment with your doctor and sign a consent form before scheduling the procedure. You will also receive comprehensive information about the treatment.
Optilume is a minimally invasive treatment for urethral strictures. It provides immediate relief and works by preventing the regrowth of scar tissue, which commonly recurs after dilations or direct visual internal urethrotomy. The last 2 are traditional treatments for urethral strictures.
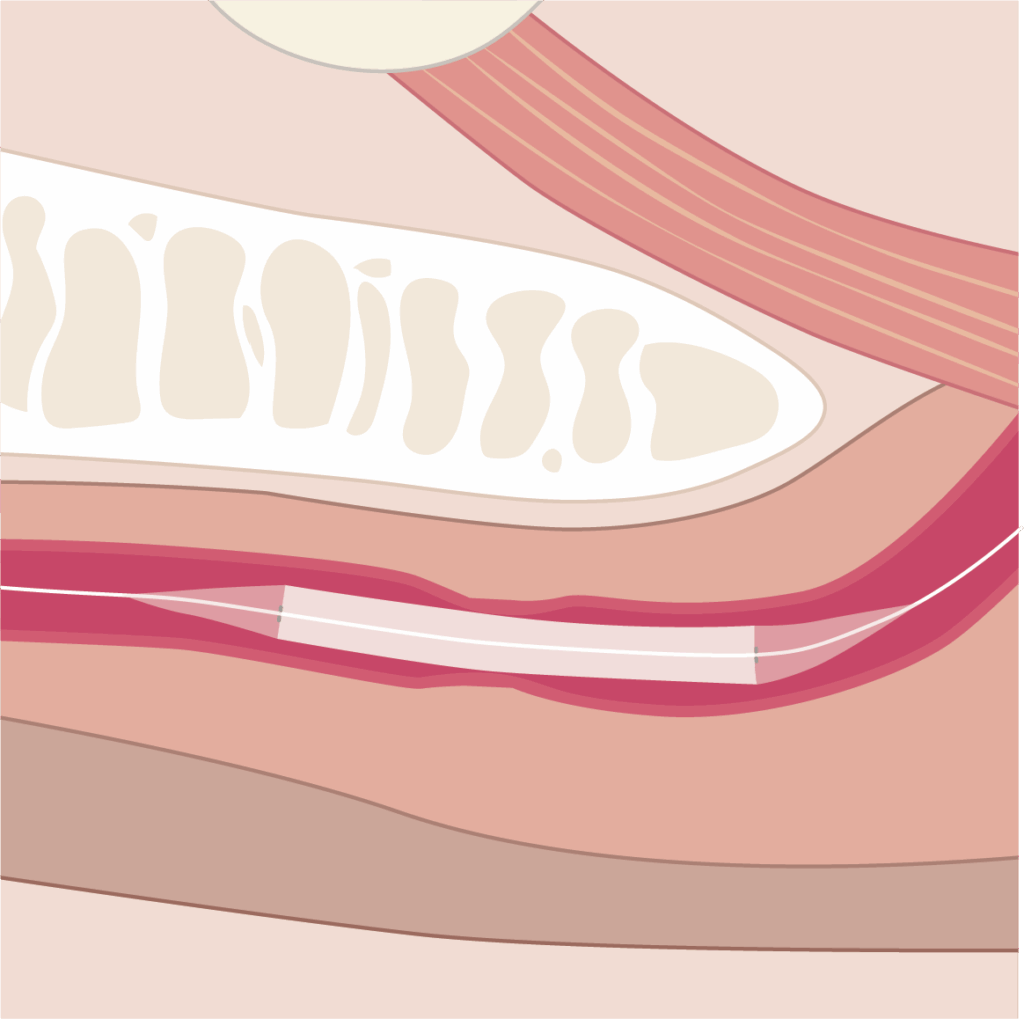
Optilume consists of a small, cylindrical balloon coated with medication, called Paclitaxel which is a medicine for cancer treatment. It is designed to both dilate the urethra and reduce the likelihood of stricture recurrence.
This procedure can be performed under:
Note: Optilume is National Institute for Health and Care Excellence (NICE) approved only for recurrent anterior urethral strictures.
Common side effects – for 1 in 10 patients to 1 in 20 patients:
Less common complications – for 1 in 20 patients to 1 in 50 patients:
Rare complications – for less than 1 in 100 patients:
Potential complications – safety has not yet been confirmed.
During Optilume treatment, the medication Paclitaxel works directly on the urethra. This means only a very small amount enters the bloodstream, so the rest of your body is unlikely to be affected. However, potential risks to your fertility and your partner’s future pregnancies cannot be entirely ruled out.
The effects of Optilume treatment on fertility and sexual function have been studied in the ROBUST III trial:
Abstain from sexual activity or use barrier contraception such as condoms for 30 days after your treatment.
If your partner/wife is of childbearing age use highly effective contraception and avoid fathering children for at least 6 months after your treatment.
If the procedure is performed under local anaesthesia, you will attend Westwood Park or the Day Case Unit at St Luke’s Hospital, as an outpatient. The treatment will be carried out in a quiet, private environment by experienced staff.
If performed under general or spinal anaesthesia, you will need to attend a pre-assessment appointment to make sure it is safe for you to have an anaesthetic. You will then receive instructions regarding when you will need to stop eating ahead of the treatment, what time you should arrive and the location.
You will be admitted to either Ward 20 at the Bradford Royal Infirmary or the Day Case Unit at St Luke’s Hospital. The nursing team will admit you and the surgical team will confirm your consent for the procedure and answer any remaining questions.
If you have concerns or wish to reconsider the procedure, please discuss them with the medical team before proceeding.
A catheter will be in place for 5–8 days.
You will return to Westwood Park Hospital for catheter removal.
After removal, you will be asked to drink water and urinate 3 times. You will have an ultrasound to check for any residual urine in your bladder. Please allow half a day for this process.
You will be followed up in clinic at:
Please, contact the Urology Secretary on telephone number: 01274 276015. Working days/hours: Monday to Friday between 8.00am and 3.00pm, except bank holidays.
Outside working hours, please attend the Emergency Department at the Bradford Royal Infirmary.
You can contact us using the Relay UK app. Textphone users will need to dial 18001 ahead of the number to be contacted.
Bradford Teaching Hospitals NHS Foundation Trust is a smoke-free organisation. You are not permitted to smoke or in use e-cigarettes in any of the hospital buildings or grounds.